London's Breast Cancer Screening Crisis: Why Are So Many Missing Vital Appointments?
The London Assembly Health Committee has launched a crucial investigation into why breast cancer screening rates in the capital remain alarmingly low compared to other UK regions. With screening coverage in London standing at just 62.8 per cent in 2024 – significantly below the NHS's acceptable threshold of 70 per cent – health experts warn that distinctive challenges are putting Londoners at risk.
The Impact of Population Churn on Screening Invitations
Dr Josephine Ruwende, Cancer Screening Lead at NHS England, told the committee that London's unique "population churn" presents a major obstacle. This phenomenon, driven by gentrification, high living costs forcing people out of the city, and a high proportion of renters frequently moving, makes it difficult for the health service to contact eligible individuals.
"The biggest factor we see in London is the impact of population churn," Dr Ruwende explained. "People change addresses and then fail to update their GP details, which directly affects the invitation process since GP records are used to identify those eligible for screening."
Even in London's most affluent boroughs, population turnover can reach 40 per cent annually. Additionally, many residents maintain second homes or spend substantial time abroad, complicating the NHS's ability to maintain accurate contact information. Consequently, screening invitations are often sent to incorrect addresses or when individuals are outside the country.
Medical Mistrust and Cultural Barriers in Diverse Communities
London's cultural diversity, while one of its strengths, also creates specific challenges in encouraging screening uptake. Leeane Graham, Advocacy Lead at Black Women Rising, highlighted deep-seated cultural barriers and medical mistrust within some ethnic minority communities.
"There's a lot of medical mistrust within the Black community, which has been ongoing for many, many years," Graham stated. "Cultural barriers, fear, and negative experiences – often shared through word of mouth – prevent some women from attending screenings."
Lee Dibben, Education and Policy Manager at Outpatients, noted similar issues within the LGBTQ+ community, where previous negative healthcare experiences have created a "trust deficit." Dibben emphasised the need for inclusive campaigns and messaging to bridge this gap.
Physical Barriers and Lack of Awareness Across All Groups
Helen Dickens, Chief Support Officer at Breast Cancer Now, warned that awareness issues extend beyond specific communities. National polling by her organisation revealed that 19 per cent of women feel uncomfortable with NHS screening of their bodies, while 10 per cent fear potential pain or harm.
"We know that for some groups of women, these fears and issues around trust and accessibility are even higher," Dickens added. "But physical barriers also play a significant role – 16 per cent of women who didn't attend screening cited transportation difficulties."
Despite London's extensive public transport network, screening centres are not available in every borough, creating accessibility challenges. Zara Gross of the South East London Cancer Alliance further noted that in deprived areas, many potential invitees cannot secure time off work, particularly those on zero-hour contracts.
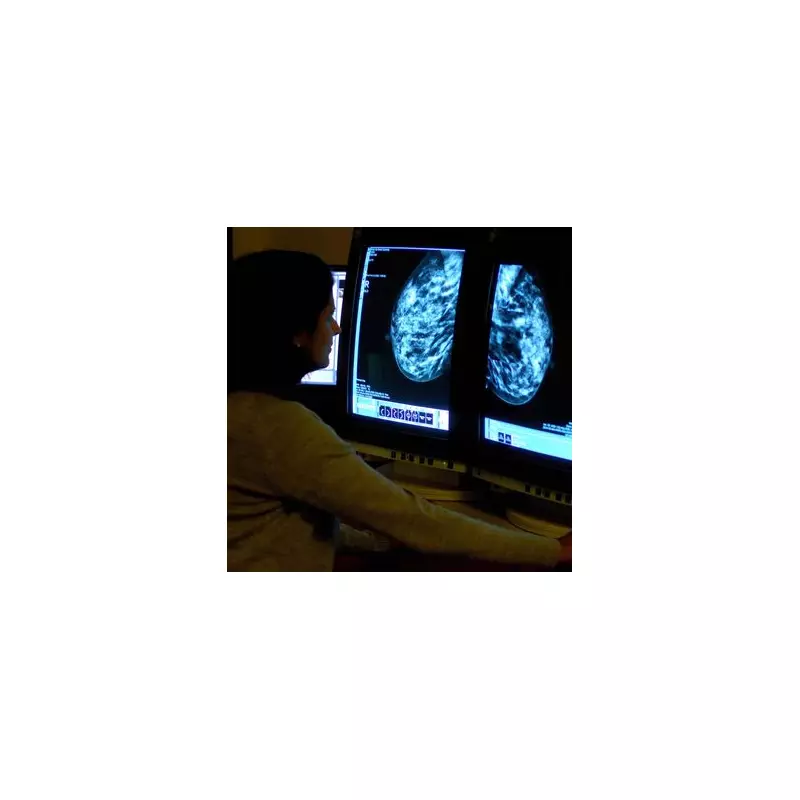
The Critical Importance of Early Detection
The low screening uptake has raised serious concerns among health professionals, who stress that early diagnosis dramatically improves survival rates. Helen Dickens highlighted the stark difference: "If you're diagnosed at stage one, your five-year survival outcome rate is 98 per cent. If diagnosed at a later stage, treatment becomes much more brutal."
Dr Will Teh, Consultant Radiologist at the North London Breast Screening Service, confirmed that non-attenders and irregular attendees tend to have cancers detected at later stages, adversely affecting their prognosis.
In response to these challenges, the NHS in London launched its first-ever breast screening campaign last year. Meanwhile, the government's new national cancer plan, set for announcement on February 4 (World Cancer Day), promises to address inequalities, though initial details suggest a focus on rural and coastal areas rather than urban centres like London.





