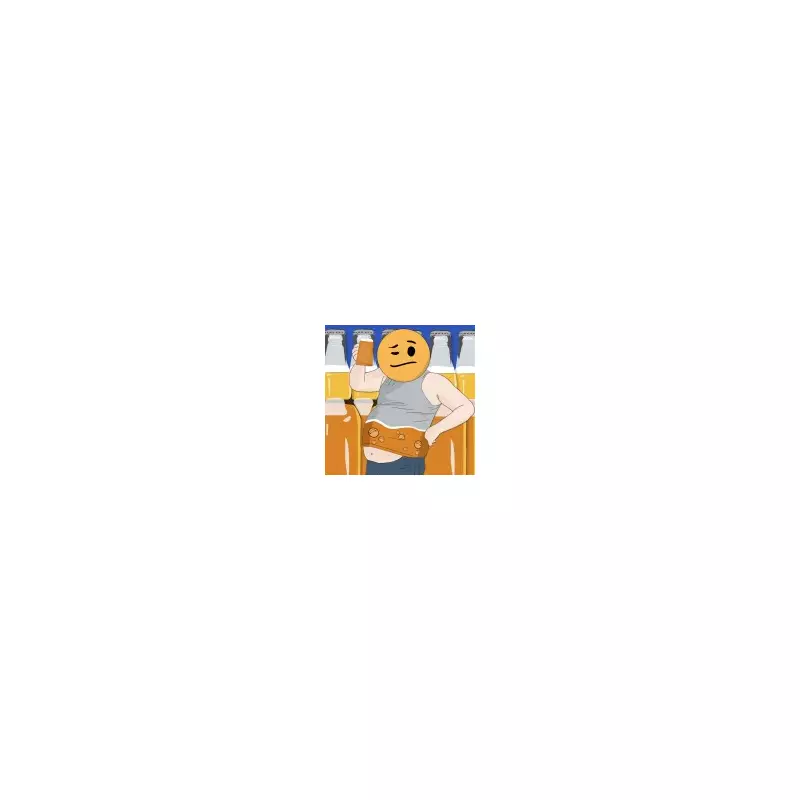
Imagine becoming legally intoxicated without consuming a single drop of alcohol. For individuals with a rare and baffling medical condition, this is a daily reality. Now, a breakthrough study has identified the specific gut bacteria responsible for this phenomenon, paving the way for new treatments.
The Mystery of Auto-Brewery Syndrome Explained
Auto-brewery syndrome (ABS), also known as gut fermentation syndrome, is a rare gastrointestinal disorder where the body produces its own alcohol. Fungi and bacteria in the gut ferment carbohydrates from starchy or sugary foods into ethanol. This internal brewing process can lead to blood-alcohol levels high enough to cause significant intoxication, memory loss, aggression, and even liver damage.
For nearly a century, the condition has been poorly understood, leading to widespread stigma and misdiagnosis. Sufferers have faced arrest for drunk-driving and accusations of being secret alcoholics, with only a few dozen official diagnoses worldwide, though the true number is believed to be higher.
Scientific Breakthrough in Bacterial Culprits
In a study published in Nature Microbiology on January 8, 2026, a team from the University of California San Diego School of Medicine made a crucial discovery. They assessed 22 people living with ABS and compared them to 21 of their partners.
The researchers found that ABS patients' stool contained significantly more ethanol. They identified that specific gut bacteria, including Escherichia coli and Klebsiella pneumoniae, were driving the alcohol production.
'These microbes use several ethanol-producing pathways and drive blood-alcohol levels high enough to cause legal intoxication,' explained medicine professor Bernd Schnabl, a study author. While these were the primary culprits, the team noted that some patients had different microbes responsible for their condition.
New Pathways to Diagnosis and Treatment
The findings, which pinpoint the exact bacterial pathways involved, open the door to revolutionary approaches for managing ABS. The research paper suggests that targeted antibiotics could be developed to inhibit the enzymes crucial to the fermentation process.
Another promising treatment is faecal microbiota transplantation (FMT). This procedure involves transferring beneficial gut microbes from a healthy donor to a patient. Remarkably, one participant in the study remained symptom-free for over 16 months after receiving two such transplants.
The team also recommends stool tests as a more effective diagnostic tool than traditional blood-alcohol testing. Elizabeth Hohmann, another study author from Mass General Brigham Department of Medicine, stated: 'Our findings may lead the way toward easier diagnosis, better treatments, and an improved quality of life for individuals living with this rare condition.'
This research not only solves a long-standing medical mystery but also offers tangible hope to those whose lives have been upended by a condition that turns a simple meal into a source of unintended intoxication.