The Silent Epidemic: How Endometriosis Goes Undiagnosed for Years
In Australia, endometriosis affects approximately one in nine women, yet the medical system routinely fails them. Diagnosis typically takes between seven to ten years, during which women's pain is minimized, normalized, or dismissed as psychological. This systemic failure becomes particularly pronounced in fertility medicine, where an industry structured around efficiency rather than comprehensive care compounds the problem.
When 'Unexplained' Means Uninvestigated
"The female body is such a mystery," a fertility specialist remarked casually during a consultation about secondary infertility. Despite describing increasingly severe monthly pain that affected daily functioning, the response was consistent across multiple specialists: the pain was treated as incidental, unrelated, and something to be endured rather than investigated.
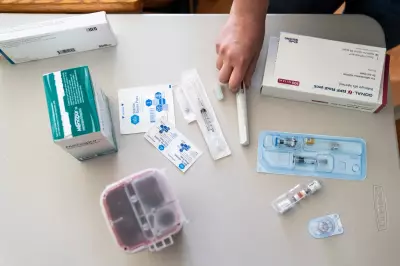
Over three years, the pattern repeated. Blood tests, charts, timelines, and always the same conclusion: unexplained secondary infertility. Medications, hormones, dietary changes, lifestyle adjustments, obsessive cycle tracking, internal ultrasounds, timed intercourse, and multiple rounds of intrauterine insemination followed. The body became a site of constant intervention while being told to relax, stay positive, and not think about it too much.
The Psychological Toll of Medical Dismissal
Each negative pregnancy test carried its own grief, but layered on top was something more insidious: the exhaustion of not being believed. The psychological burden of being told, implicitly or explicitly, that suffering is unrelated, irrelevant, or simply "one of those things" creates a unique form of trauma.
In vitro fertilization was presented as the logical next step—efficient, protocol-driven, almost inevitable. Yet something resisted: a gut feeling, quiet but insistent, that fundamental issues were being overlooked. That the pain mattered. That the body was trying to communicate something important.
The Turning Point: Listening to Women's Pain
The breakthrough came from hearing an obstetrician-gynaecologist challenge the concept of "unexplained infertility," suggesting it often means the investigative work simply hasn't been done. This perspective gave shape to what had been felt all along: something had been missed.
One final consultation brought a different response. After describing pain that now significantly impacted work and daily functioning, the specialist paused, listened, and casually suggested a laparoscopy. Within a month, surgery revealed extensive endometriosis—some wrapped around nerves and forming its own blood supply. What was expected to be straightforward took far longer than anticipated.
The Devastating Revelation
The discovery was both devastating and vindicating. There it was—the physical reality felt in the body all along, finally named. The mystery evaporated instantly. The infertility was no longer "unexplained"; it had simply been ignored.
This moment brought complex emotions: relief and gratitude sat alongside grief so sharp it took breath away. Grief for years lost to pain, for work opportunities that slipped away when the body couldn't conform to timelines assuming women's bodies won't interrupt progress, for emotional whiplash of hope and despair repeating monthly.
Systemic Failures in Women's Healthcare
Endometriosis statistics reveal a healthcare crisis. With one in nine Australian women affected and diagnosis delays averaging seven to ten years, women's pain is routinely minimized. In fertility medicine, this dismissal combines with an industry structured around efficiency and throughput rather than curiosity and comprehensive care.
IVF itself isn't the problem—for many, it's life-changing and essential. But when it becomes the default response before thoroughly investigating underlying causes, it risks becoming a conveyor belt system. Women become processed rather than heard; symptoms become managed rather than understood.
'Unexplained' as Diagnostic Failure
"Unexplained" isn't a diagnosis—it's a failure of imagination, time, or willingness to investigate thoroughly. When women's pain is repeatedly minimized across medicine, work, and systems designed for efficiency rather than care, something must signal that harm has occurred.
Sometimes that signal is anger—not as overreaction but as evidence. Not something to be soothed away but something asking to be examined. Anger for oneself and for countless women still being told gently, confidently, that their bodies are mysteries. They're not mysteries—they simply deserve to be listened to.
The journey to pregnancy brought gratitude but didn't erase the cost of getting there. What remains is the knowledge that without trusting instincts and refusing to accept "mystery" as an answer, the waiting might have continued indefinitely. The female body isn't mysterious—it's systematically misunderstood and inadequately investigated.