A silent but ferocious health crisis is sweeping across the United Kingdom, marked by relentless itching, sleepless nights, and a profound sense of isolation. Scabies, an infestation caused by microscopic mites that burrow under the skin, has seen a dramatic and worrying surge in cases, leaving a trail of distress in its wake.
The Personal Toll of a National Outbreak
For Louise, a 44-year-old mother from south-west England, the battle against scabies became an all-consuming nightmare. After telltale spots appeared on her and her children in September, her life descended into a frantic cycle of medical treatments and exhaustive decontamination. Two rounds of topical permethrin cream failed to stop the infestation, despite washing laundry after every use, steaming soft furnishings, and quarantining belongings in bin bags.
"It was hell," she confesses. "My mental health was in the pan, the scratching, the itching drives you insane... I wouldn't wish it on my worst enemy." In a final, desperate move, her family evacuated their home last November, renting a caravan for a week while undergoing a third round of treatment. Her experience, while extreme, echoes a growing desperation found in countless social media pleas from others trapped in the same itchy purgatory.
Understanding the Scabies Surge: Facts and Figures
This is not a relic of the past. Data reveals a sharp and sustained increase in scabies diagnoses across the country. A 2024 report from the UK Health Security Agency (UKHSA) analysed cases presenting at sexual health services and found a staggering 44% increase between 2023 and 2024, rising from 3,393 to 4,872 cases. This is a dramatic jump from the pre-pandemic average of around 1,500 annual cases.
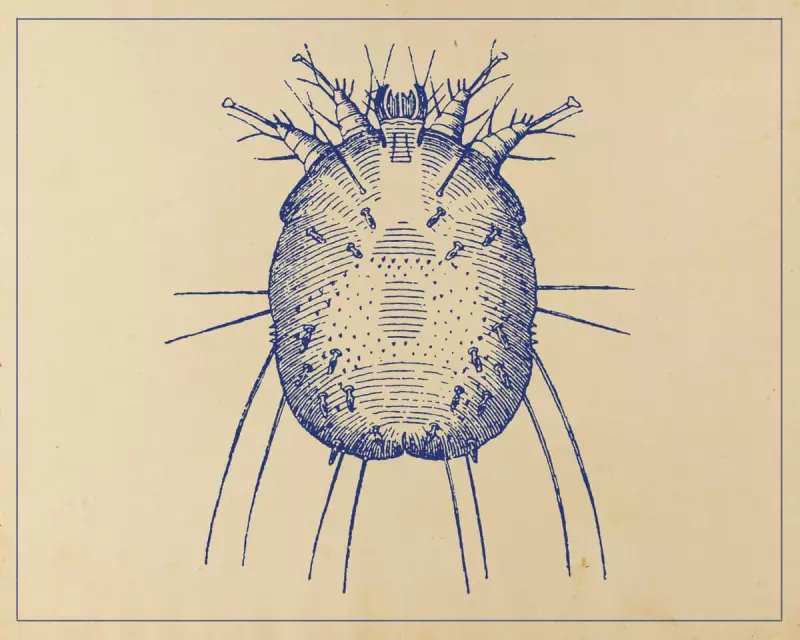
Similarly, surveillance by the Royal College of General Practitioners shows cases remain stubbornly higher than the five-year average, peaking at almost double the usual rate in the final four months of 2023. The north of England is particularly affected. The mites, Sarcoptes scabiei var hominis, are spread through prolonged skin-to-skin contact and can survive on surfaces for up to 36 hours, making outbreaks in households and communal living spaces notoriously difficult to contain.
Treatment Challenges and Systemic Hurdles
Experts are grappling with the reasons behind the outbreak. Dr Donald Grant, a GP and senior clinician at The Independent Pharmacy, points to a potential "ping-pong" effect of reinfestation, exacerbated by past shortages of first-line treatments like permethrin and malathion due to supply chain issues.
Professor Michael Marks of the London School of Hygiene & Tropical Medicine notes similar trends across Europe. He suggests outbreaks in crowded settings like university halls, combined with delays in accessing GP care and inadequate contact tracing, are likely contributors. "Probably all of this plays a role," he states.
While there is talk of drug resistance, Professor Marks emphasises that most treatment failure is due to "pseudo-resistance"—the immense practical difficulty of correctly applying cream over the entire body for the required 12 hours and ensuring all close contacts are treated simultaneously. This is compounded by the intense shame associated with the condition, which Dr Lea Solman, a consultant paediatric dermatologist, identifies as a major obstacle to controlling outbreaks.
A Crisis Disproportionately Affecting the Young
The data indicates that young adults are bearing the brunt of the outbreak. The UKHSA report found that 41% of 2024 diagnoses were in people aged 20 to 24. For students like John, a 20-year-old in London, the infestation has been devastating. "My sleep has taken such a blow and I’m going a bit loopy," he says, describing blood-stained sheets and significant scarring from scratching. The financial burden of constant laundry is also crippling for those on tight budgets.
Professor Tess McPherson of the British Association of Dermatologists confirms that university freshers' week has become a peak transmission time, with some students attempting treatment up to ten times or even leaving their studies. The consequences of unchecked scratching can be serious, potentially leading to skin infections and, in rare cases, renal disease.
As sufferers like Louise continue their recovery, hoping the dreaded "post-scabies itch" is the final chapter, the UK faces a complex public health challenge. The combination of a highly contagious parasite, practical treatment hurdles, systemic pressures on the NHS, and a debilitating stigma has created a perfect storm, making the humble scabies mite a formidable modern-day foe.





